Cory:
Unlock Your AI Assistant Now!
We are performing transcatheter aortic valve implantation (TAVI) procedures better than ever. Technical advancements and operator expertise have led to improved outcomes, and this, combined with growing evidence supporting TAVI durability, has accelerated its adoption in younger patients with longer life expectancy. But this progress comes with a caveat: longer post-TAVI survival means an increasing need for coronary angiography, percutaneous coronary intervention (PCI), and valve reintervention, all of which depend on reliable coronary cannulation (CC)1. In 2020, Barbanti et al2 reported that selective coronary re-engagement was unsuccessful in 7.7% of patients after TAVI with the Evolut R/PRO valve (Medtronic), identifying implant depth and transcatheter heart valve (THV) oversizing relative to the sinus of Valsalva as predictors of failure. At that time, commissural and coronary alignment were rarely a concern during implantation. Subsequent studies recognised that misalignment might be a key driver of difficult CC, sparking device iterations and procedural refinements aimed at improving alignment – and, consequently, coronary access. In this issue of EuroIntervention, the study by Ohno et al3 confirms that these efforts are bearing fruit. Their multicentre prospective study demonstrates that commissural alignment, defined according to ALIGN-TAVR Consortium standards4, was achieved in 86.4% of patients treated with the Evolut FX valve (Medtronic), while CC was successful in 100% of left coronary artery (LCA) cases and 96.7% of right coronary artery (RCA) cases. These are clear improvements over prior reports, including the contemporary CAvEAT Registry, where moderate or severe commissural misalignment was still seen in nearly one-third of cases5. Ohno and colleagues deserve credit for their rigorous methodology, including systematic post-TAVI computed tomography and intraprocedural CC in all patients, and for using uniform definitions from ALIGN-TAVR4. Their results reflect a meaningful advancement in both technology and procedural practice. But despite these gains, several issues remain (Figure 1). First, while commissural alignment rates were high, coronary misalignment (moderate or severe) was still present in approximately 20% of patients. No strategies to improve coronary alignment per se are currently implemented in routine practice. Given that coronary alignment, rather than commissural alignment alone, is the most predictive factor for CC feasibility and efficiency, this remains a key unmet need. Second, the focus of this and similar studies has been on CC after an index TAVI procedure, but redo-TAVI (transcatheter aortic valve [TAV]-in-TAV) will inevitably become more common as this younger TAVI population ages. In patients at risk for coronary obstruction during reintervention, coronary misalignment can preclude the use of leaflet modification techniques such as Bioprosthetic or native Aortic Scallop Intentional Laceration to prevent Iatrogenic Coronary Artery obstruction (BASILICA)67. New dedicated leaflet laceration devices may help in patients with eccentric coronary ostia, but they are not yet commercially available. Third, while successful CC is essential, it does not guarantee that PCI itself can be safely and effectively performed. Procedural support and equipment manipulation may be hampered even after successful ostial engagement. In a prior analysis by Won-Keun et al, nearly half of acute coronary syndromes post-TAVI remained untreated despite a high rate of CC8. Data on PCI success rates in patients with commissural alignment strategies are still lacking, but they will surely become a topic of intense investigation. In sum, this study demonstrates that the combination of new-generation THV design and contemporary procedural practice has led to impressive CC success rates: 100% for the LCA and 96.7% for the RCA. This was achieved even before the introduction of the Evolut FX+ platform (Medtronic), which promises further facilitation of coronary access by incorporating enlarged frame cells. Yet, moderate-to-severe coronary misalignment remains frequent, highlighting a critical limitation of our current approach. As TAVI expands further into younger populations, ensuring lifetime coronary access becomes an essential procedural goal. The field now requires a next step: dedicated procedural strategies or device designs specifically aimed at optimising coronary alignment, not just commissural alignment. Moreover, research should extend beyond CC feasibility to examine PCI success rates and procedural safety in these patients, including in the context of future TAV-in-TAV procedures. While the achievements documented by Ohno et al represent substantial progress, they also expose the need for additional innovation. Our pursuit of perfection in TAVI alignment is not yet complete. 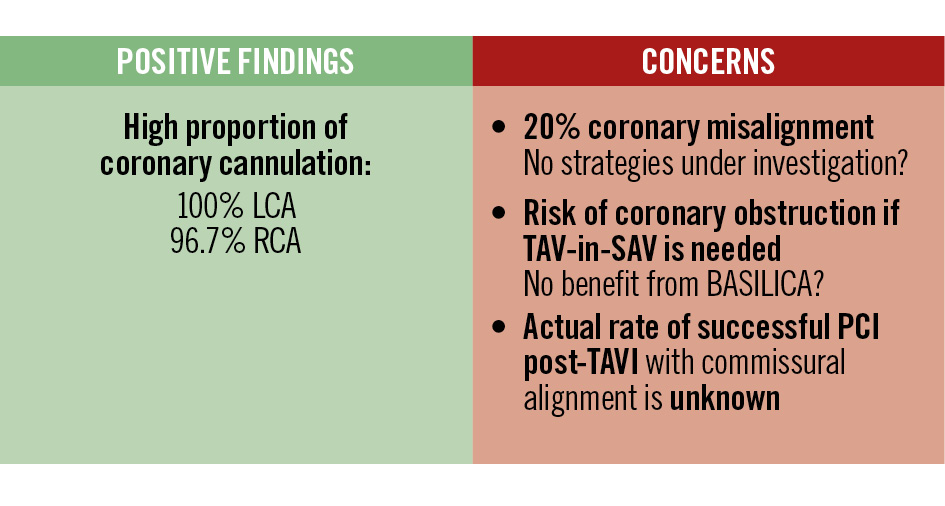
Figure 1. Summary of the main findings and concerns regarding commissural and coronary alignment following TAVI with the Evolut transcatheter heart valve. BASILICA: Bioprosthetic or native Aortic Scallop Intentional Laceration to prevent Iatrogenic Coronary Artery obstruction; PCI: percutaneous coronary intervention; RCA: right coronary artery; SAV: surgical aortic valve; TAV: transcatheter aortic valve; TAVI: transcatheter aortic valve implantation
Conflict of interest statement
I. J. Amat-Santos is a proctor for Boston Scientific, Medtronic, Meril Life Sciences, and Microport. F. Pensotti has no conflicts of interest to declare.