Cory:
Unlock Your AI Assistant Now!
Arterial hypertension is highly prevalent in patients with chronic kidney disease (CKD)1. Sustained high blood pressure (BP) accelerates kidney function decline, which in turn makes hypertension difficult to treat, and renal sympathetic signalling may negatively impact kidney function and BP1. Renal denervation (RDN) aims to disrupt this circuit with beneficial effects on BP control and, theoretically, kidney function. Despite the strong rationale for RDN use in patients with CKD, these subjects are frequently excluded from randomised controlled trials, and the European Society of Cardiology (ESC) guidelines contraindicate RDN if the estimated glomerular filtration rate (eGFR) is below 40 mL/min/1.73 m1,2]. As early RDN adopters, we collected data to explore the medium- to long-term effects of this therapy on BP and kidney function in subjects with various degrees of CKD. Patients with resistant and/or uncontrolled hypertension were screened for RDN, as approved by the local institutional review board. Eligibility and enrolment were assessed by the dedicated multidisciplinary team as described previously2. Clinical evaluation, blood and urine tests, and abdominal imaging ruled out secondary hypertension, and preliminary medical therapy optimisation was conducted. Resistant hypertension was defined as office blood pressure (OBP) >140/90 mmHg despite at least three antihypertensive drugs, including a diuretic, at the maximum tolerated dose12. Uncontrolled hypertension was defined as BP over the target without the possibility of further therapy implementation. Ambulatory blood pressure monitoring (ABPM) for 24 hours ruled out white coat hypertension12. Kidney function was assessed through serum creatinine and eGFR (CKD Epidemiology Collaboration [CKD-EPI] equation)34. CKD was defined as an eGFR ≤60 mL/min/1.73 m2,4. RDN procedures were performed by trained interventional cardiologists with radiofrequency (RF) devices (unipolar Symplicity Flex catheter, later replaced by the quadripolar Spyral catheter [both Medtronic]). Ablations were bilaterally delivered, both in the main renal arteries and in suitable branches with diameters between 3 mm and 8 mm, according to the protocol2. High-flow hydration was provided to all patients 24 hours before and after the procedure. Contrast-induced acute kidney injury (CI-AKI) was defined by an absolute creatinine increase of>0.3 mg/dL within the 48 hours post-procedure2. The primary endpoints explored procedural safety and BP reduction. A) Safety: absence of major vascular complications (renal artery perforation or dissection, embolic events, major bleeding, kidney failure, stroke, myocardial infarction, any cause of death) within one month. B) BP reduction: assessed through ABPM and OBP at 12, 24, and 36 months. The secondary endpoints were kidney function in the long term and changes in antihypertensive medications. Continuous variables are presented as mean and standard deviation (SD) and compared using paired t-tests. Categorical data are expressed as numbers and percentages, and were compared using the chi-square test. We included 100 patients (75% males) between 2013 and 2023. Of them, 22 patients had stage 1 CKD, 26 stage 2, 19 stage 3a, 14 stage 3b, 7 stage 4, and 12 stage 5 under renal replacement therapy (RRT)4. Baseline characteristics are shown in Supplementary Table 1. Five patients developed CI-AKI, with subsequent recovery. Three patients developed a femoral pseudoaneurysm requiring embolisation. The eGFR showed a non-significant decrease at three years, regardless of the stage of CKD (p>0.05) (Figure 1). The mean (SD) annual decline in eGFR was 1.12 (0.28) mL/min/1.73 m². Patients under RRT were excluded from the eGFR trend analysis. A significant and sustained (up to three years) reduction of BP values was observed in all classes of CKD (p<0.05). Importantly, BP improvement allowed six patients on RRT to successfully undergo kidney transplant. Two CKD stage 4 patients (eGFR 23 mL/min/1.73 m² and 29 mL/min/1.73 m², BP reductions of 10 mmHg and 28 mmHg at 3 years) required RRT approximately two years after RDN, without AKI occurrence at the time of RDN. Similar trends in BP reduction were observed in males and females. The number of antihypertensive medications per day tended to decrease after RDN, confirming that the effect of RDN does not depend on a heavier drug burden (Supplementary Table 2, Supplementary Table 3, Supplementary Figure 1). This study adds reassuring data to the clinically relevant and frequently debated question regarding RDN therapy in patients with reduced GFR. Our main findings are as follows: 1) RF-RDN is safe and effective in selected hypertensive patients regardless of the presence and degree of kidney dysfunction. 2) RDN may slow down kidney function decline over time, which can prove especially beneficial among patients with established CKD. 3) Despite the lack of a control arm, the observed eGFR decline at 3 years was lower than expected (2 mL/min/1.73 m2/year). Randomised studies should be considered to assess whether blood pressure lowering with RDN can be renoprotective in low-GFR hypertensive subjects. Our data aligned with the Global Simplicity Registry5. We acknowledge several limitations: the data are derived from a single-centre experience; detailed follow-up data for medical therapies are not available for all patients; and data on other parameters, such as cystatin-c or albuminuria and urine albumin/creatinine ratio, were available only in a minority of subjects and were not considered. In conclusion, RF-RDN can be safe and effective in selected patients with CKD, with long-term benefits that extend beyond BP reduction. A slowing down of kidney function decline in any degree of pre-existing kidney disease emerged from our experience. If larger studies support our findings, guidelines should reconsider the restrictions on performing RDN in patients with CKD. 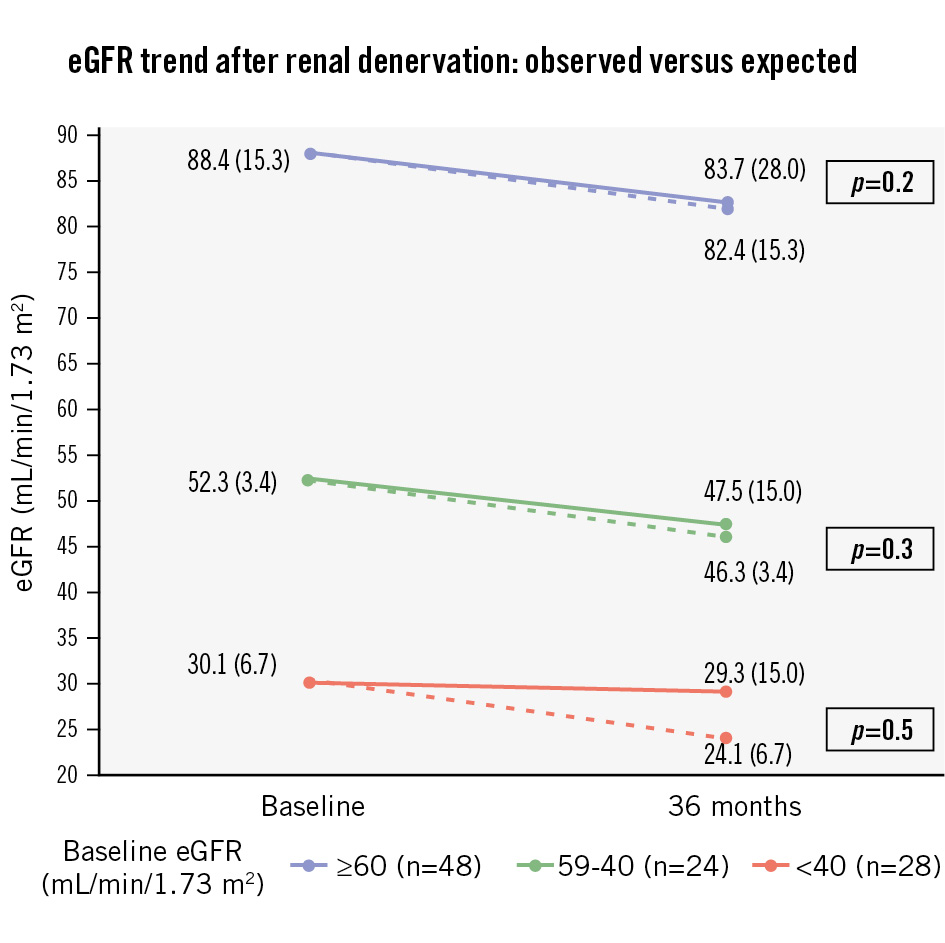
Figure 1. Trend of kidney function after renal denervation at three years of follow-up. Values of eGFR are expressed as mean (SD). The continuous lines represent the mean (SD) observed eGFR at follow-up, for each group we considered (eGFR ≥60, 59-40, <40 mL/min/1.73 m2). Dashed lines represent the expected mean (SD) eGFR, considering an estimated physiological mean reduction of 2 mL/min/1.73 m2/year for patients with hypertensive nephropathy. The observed mild eGFR decline was lower than expected in each subgroup. Even though statistically non-significant (p>0.05), this may suggest a possible slowing-down effect on the progression of kidney dysfunction, related to a reduction of blood pressure values and a decrease in the excessive adrenergic activation that typically characterise patients with CKD. CKD: chronic kidney disease; eGFR: estimated glomerular filtration rate SD: standard deviation
Conflict of interest statement
F. Ribichini declares consulting fees and payments of honoraria from Medtronic. G. Gambaro declares payment of honoraria from Medtronic. The other authors have no relevant conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.