Cory:
Unlock Your AI Assistant Now!
Abstract
Background: Despite excellent long-term results, patients who have undergone valve-sparing root repair (VSRR) or a Bio-Bentall procedure may require a future secondary valve-related intervention.
Aims: We aimed to assess the feasibility of transcatheter valve-in-root procedures in patients who have previously undergone either a VSRR or a root replacement with a Bio-Bentall, in anticipation of lifetime management.
Methods: Between 2012 and 2022, 537 patients underwent a VSRR or a Bio-Bentall procedure in our institution. In 363 patients, a postoperative computed tomography angiography was available (VSRR n=250; Bio-Bentall n=113) to evaluate the feasibility of a transcatheter valve-in-root implantation. Annulus area, annulus-to-coronary distance, coronary ostium size, and the valve-to-coronary distance (VTC) were measured using dedicated software.
Results: After VSRR, 4.8% of patients had an annulus area over 840 mm2, thus being unsuitable for a valve-in-root procedure. In 12.4% of cases after a Bio-Bentall procedure, the annulus area was below 300 mm2, which complicates valve-in-root implantation due to potential patient-prosthesis mismatch. The annulus-to-coronary distance for both coronary arteries was significantly higher after VSRR compared to Bio-Bentall (right coronary artery: 18.0±5.8 mm vs 12.5±5.4 mm; p<0.001; left coronary artery [LCA]: 11.6±4.6 mm vs 8.0±4.5 mm; p<0.001). Out of a total of 98 coronary ostia located below the upper frame level, 63.3% had a VTC below 4 mm. The VTC to the LCA was significantly larger after Bio-Bentall with a Valsalva graft, with a median of 4.95 (interquartile range [IQR] 4.2-5.9) mm compared with 3.1 (IQR 2.3-4.2) mm (p<0.001) in patients who had a straight graft implanted.
Conclusions: The feasibility of a future transcatheter valve-in-root procedure depends on the anatomical conditions of the aortic root after the initial operation. A high reimplantation of coronary ostia, the choice of the vascular graft, and a foresighted valve sizing may facilitate a future transcatheter valve-in-root implantation.
Surgical results after valve-sparing root repair (VSRR) or a Bio-Bentall procedure are excellent, with 10-year freedom from reoperation ranging between 80% and 96%123. However, due to the ageing population and the patient-driven request for biological valves even at a younger age, the probability of a secondary valve-related intervention is likely and needs to be considered for a patient’s lifetime management.
Transcatheter valve-in-valve (ViV) procedures are increasingly utilised in patients requiring redo-valve interventions for structural degeneration of biological valve prostheses, with convincing short- and midterm results over the last decade45. Parameters supporting an uncomplicated transcatheter aortic valve implantation (TAVI) after surgical aortic valve replacement (SAVR) exist and include, among others, the type and size of the initial aortic valve prosthesis to avoid patient-prosthesis mismatch (PPM), a sufficient annulus-to-coronary distance, and a sufficient valve-to-coronary distance (VTC) to avoid coronary obstruction67.
A Bio-Bentall procedure comprises the replacement of the aortic root with reimplantation of both coronary arteries. The current surgical standard technique for a Bio-Bentall procedure involves the combination of a conventional biological aortic valve prosthesis sewn in a straight vascular graft or a Valsalva prosthesis89. Recent developments like extra-large transcatheter valves and evolving techniques, including the Bioprosthetic Aortic Scallop Intentional Laceration to prevent Iatrogenic Coronary Artery obstruction (BASILICA) manoeuvre and coronary chimneys, facilitate the treatment of technically difficult transcatheter ViV procedures and might be applicable also for patients after a Bio-Bentall or VSRR procedure101112. Although the instructions for use of the two most frequently used transcatheter aortic valves, SAPIEN 3 (Edwards Lifesciences) and Evolut FX (Medtronic)1314, do not specifically include implantation after an aortic root procedure, small patient cohorts can be found in the literature that have undergone a valve-in-root implantation15.
Considering these developments of transcatheter techniques, the surgical community should already anticipate the need for secondary interventions during the initial procedure. In the context of lifetime management, we aimed to evaluate the feasibility of a potential, later valve-in-root procedure using established parameters from computed tomography (CT) scans.
Methods
Ethical statement
This retrospective study with the identification number 24-1310-S1-retro was approved by the local ethics committee of the university hospital on 15 August 2024, and informed consent was waived.
Study design
Our study was initially designed to evaluate patients for potential valve-in-root procedures following any root operation. From January 2012 to December 2022, 760 patients underwent either a Bio-Bentall procedure or VSRR using the David technique in a single centre. All patients over the age of 18 were included. Bentall procedures using mechanical valves (n=223) were excluded since the choice of this valve does not allow for further valve-in-root treatment. In addition, patients with a missing postoperative electrocardiogram (ECG)-gated CT angiography (CTA) scan of the thoracic aorta (n=174) were excluded, resulting in 363 patients with either Bio-Bentall or VSRR (Figure 1). The CTA scans were obtained before discharge or during the first two years (after 6, 12, or 24 months) in the context of the routine postoperative follow-up.
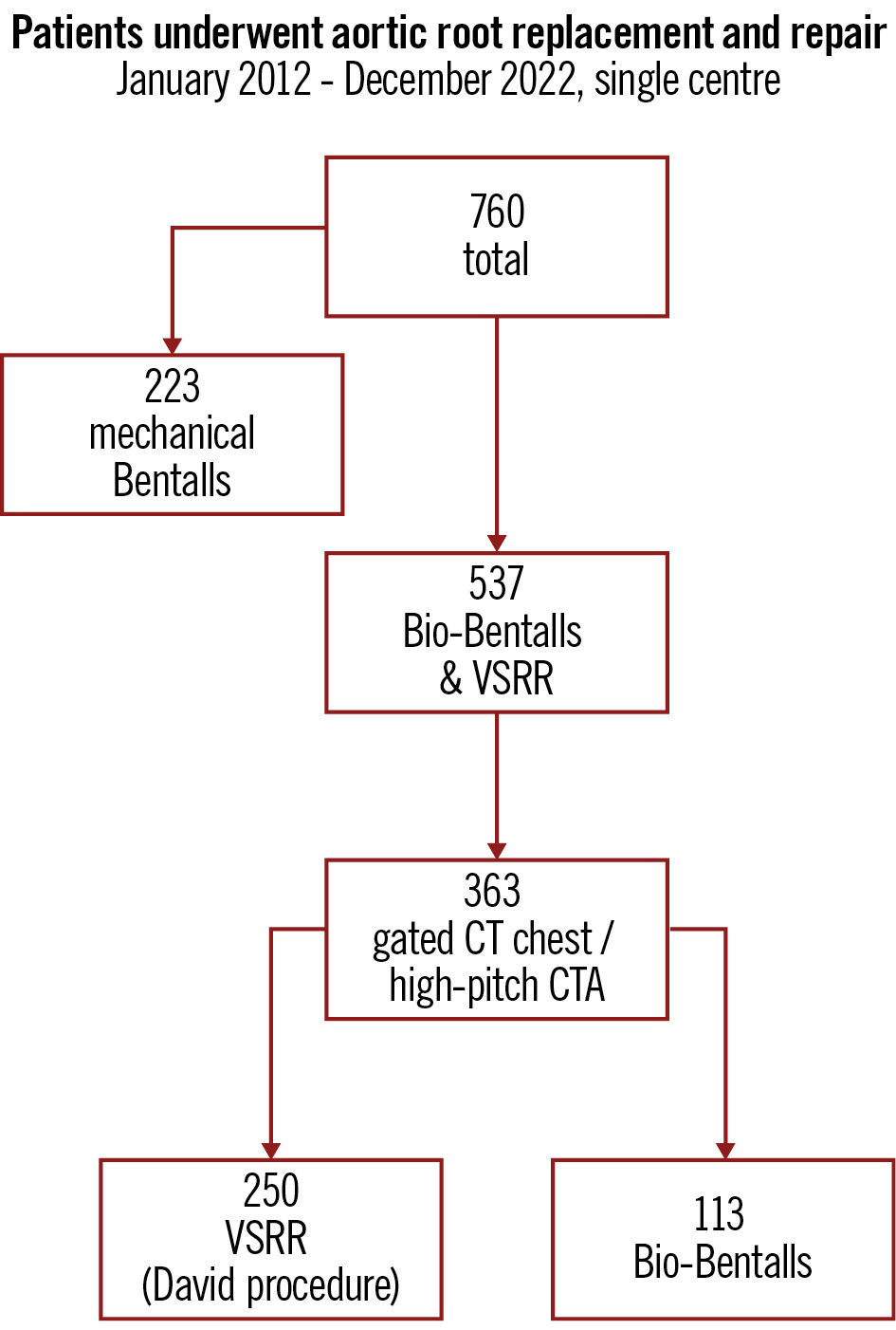
Figure 1. Study flowchart. Number of patients after Bio-Bentall or valve-sparing root repair resulting in 363 patients who were eligible for study inclusion. CT: computed tomography; CTA: computed tomography angiography; VSRR: valve-sparing root repair
Data collection
An anonymised spreadsheet form was used for data collection. Demographic, preoperative, and postoperative data were collected for all patients. Clinical covariates and operative data were automatically extracted from the clinical database.
Surgical technique
The techniques for VSRR and Bio-Bentall procedures are shown in Figure 2A and Figure 2B, respectively. After establishing cardiopulmonary bypass and cross-clamping, the ascending aorta is incised. Both coronary arteries are mobilised and dissected from the aortic root. Next, the sinus portions are excised including the dilated parts of the root, leaving the three commissures in place. For VSRR, the aortic valve is inspected and, depending on the mechanism of regurgitation, further leaflet repair is performed, i.e., leaflet plication or closure of a fenestration. For the Bio-Bentall procedure, the aortic valve is excised and the annulus debrided in case of calcifications, followed by the sizing of a biological aortic valve prosthesis. Non-everted and everted pledgeted sutures are placed along the aortic annulus, and the combination of the aortic graft and valve is created at a back table by fixing the valve to the aortic graft with three 5-0 Prolene sutures. The conduit is then sewn in, followed by anastomosis of the left and then the right coronary ostium using Prolene 5-0. For VSRR, the root reimplantation technique was carried out by reimplanting the valve into an aortic prosthesis16. The choice of using a straight or Valsalva graft remained at the discretion of the surgeon in both root repair and replacement.
In contrast to a straight tubular graft, the Valsalva prothesis has two portions. Starting with a short tubular collar of 2 cm, which is removed before implantation, the main part consists of an onion-shaped graft mimicking the sinus portion of an aortic root. At the height of the sinotubular junction, the graft becomes straight for the anastomosis with the ascending aorta. The coronary ostia are anastomosed into the onion-shaped main part, theoretically allowing for a larger distance from the biological valve9. This difference is shown in the Central illustration C.
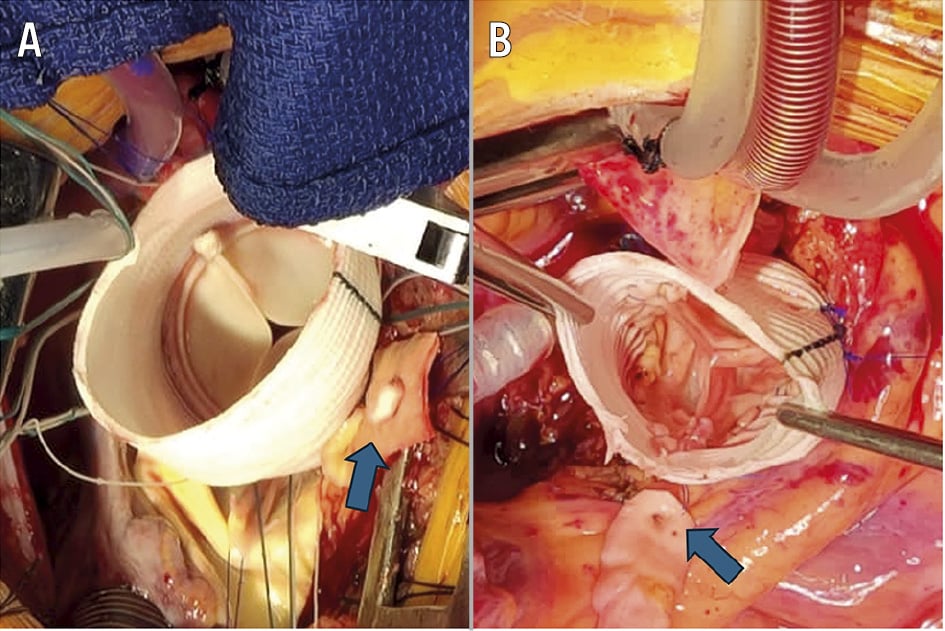
Figure 2. Intraoperative view of both procedures. A) Bio-Bentall procedure with a straight graft and a biological aortic valve prosthesis; (B) valve-sparing root repair showing the native valve inside the straight graft in a reconstructed fashion; for both images, the right coronary ostium is indicated with a blue arrow.
Computed tomography measurements
Electrocardiogram-gated CTA scans with a 0.75 mm slice thickness were obtained from patients after VSRR and Bio-Bentall procedures. These scans were assessed using the 3mensio Aortic Valve software, version 10.1 (Pie Medical Imaging) (Figure 3). Before carrying out the measurements, markers for the alignment of the aortic root and ascending aorta were manually placed. The annulus area was measured for both groups. In patients who underwent a Bio-Bentall procedure, the area of the annulus was defined as the ring of the initial aortic valve prosthesis. The coronary ostia were measured at their lowest and highest points to define partial or full position below the valve level and to calculate the size of the ostium. For assessment of the annulus-to-coronary distance, also defined as the coronary height, the lower edge of the coronary ostium was specifically chosen in the VSRR group, using a distance of 10 mm as a benchmark and orientation point to distinguish between patients at risk for coronary obstruction and those at low or no risk.
The VTC was assessed after Bio-Bentall implantation in patients who had at least one coronary partially below the level of the valve. The VTC was calculated by adding a virtual valve into the bioprosthetic frame at the level of the upper crown of the bioprosthetic valve prosthesis if the coronary ostium was partially or fully below the upper crown level.
Following Bio-Bentall implantation, patients with coronary arteries partially or fully below the upper valve frame with a VTC below 4 mm were considered complex cases. These patients were analysed separately by a highly experienced interventional cardiologist to assess the potential need for additional leaflet modification techniques, such as the BASILICA manoeuvre or coronary chimneys, in case of a future valve-in-root procedure.
A risk for coronary obstruction was defined if the VTC was below 4 mm, according to the Vancouver approach17. The impact of Valsalva versus straight graft on VTC was evaluated for patients after Bio-Bentall.
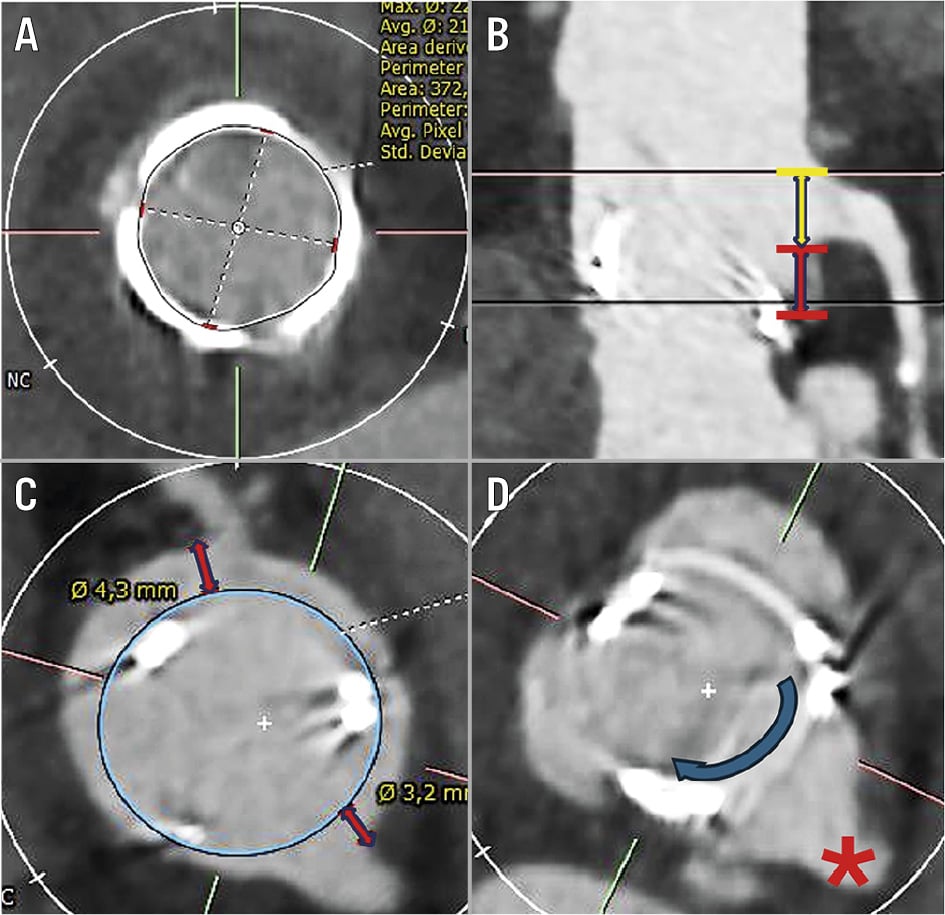
Figure 3. Parameters for potential valve-in-root implantation. A) CT measurements of the annulus area; (B) the coronary height (red bar) and coronary ostium size (yellow bar); (C) virtual valve-to-coronary distance; (D) localisation of the coronary ostium; the artificial annulus of the bioprosthetic valve appears to be visible almost at the same plane as the coronary ostium (*). CT: computed tomography
Statistical analysis
The statistical assessment was carried out with StatsDirect statistical software, version 3.3.6 (StatsDirect). Nominal and categorical variables were analysed with crosstabs and the chi-square test, and in case of small numbers, the Fisher-Freeman-Halton exact test was used. Continuous variables were checked for normal distribution using the Shapiro-Wilk test. As most of them were not normally distributed, analyses were performed with the Mann-Whitney U test. Possible correlations between numerical variables were tested for linear correlation and rank correlation using Kendall’s and Spearman’s correlation tests.
Results
Patient characteristics
Two cohorts were compared consisting of patients who had undergone VSRR (n=250) or Bio-Bentall (n=113) procedures. Patients after Bio-Bentall implantation were older (65 [IQR 59-72] years vs 54 [IQR 45-64] years; p<0.0001) and more often underwent surgery for endocarditis, type A dissections, or as a reoperation, resulting in a significantly higher European System for Cardiac Operative Risk Evaluation (EuroSCORE) II (Table 1).
Table 1. Basic characteristics of patients after VSRR or Bio-Bentall procedures.
| VSRR n=250 | Bio-Bentall n=113 | p-value | |
|---|---|---|---|
| Female | 49 (19.6) | 22 (19.5) | >0.99 |
| Age, years | 54 (45-64) | 65 (59-72) | <0.001 |
| Indication | |||
| Aneurysm | 224 (89.6) | 91 (80.5) | |
| Dissection | 24 (9.6) | 16 (14.2) | |
| Endocarditis | 2 (0.8) | 6 (5.3) | 0.01 |
| Urgency | |||
| Elective | 227 (90.8) | 90 (79.6) | |
| Urgent | 6 (2.4) | 8 (7.1) | |
| Emergency | 17 (6.8) | 15 (13.3) | 0.01 |
| Reoperation | 16 (6.4) | 25 (22.1) | <0.001 |
| EuroSCORE II | 1.6 (1-2.1) | 2.2 (1.3-3.7) | <0.001 |
| Size of aortic graft# | |||
| Small | 7 | 51 | |
| Medium | 96 | 45 | |
| Large | 147 | 17 | |
| Valsalva graft | 23 (9) | 113 (19) | |
| Data are presented as n (%), median (IQR) or n. #Aortic graft sizes were defined as 22-26 mm for small, 28-30 mm for medium, and 32-34 mm for large grafts. EuroSCORE: European System for Cardiac Operative Risk Evaluation; IQR: interquartile range; VSRR: valve-sparing root repair | |||
Distribution of graft and valve sizes
The different sizes of aortic grafts were summarised into three categories: small, including grafts of 22-26 mm; medium, 28-30 mm; and large, 32-34 mm. In the repair group, 23 out of 250 patients (9%) received Valsalva grafts, whereas in the Bio-Bentall group, Valsalva grafts were used in 22 out of 113 patients (19%). The distribution of the sizes and types of aortic grafts is illustrated in Table 1. The implanted valve types included 67 Magna Ease prostheses (Edwards Lifesciences), 5 INSPIRIS RESILIA prostheses (Edwards Lifesciences), 40 Labcor Bio-Conduits (Labcor), and 1 Mitroflow prosthesis (LivaNova), which was the only valve type in the cohort with externally mounted leaflets. The distribution of the valve sizes in the Bio-Bentall group was as follows: 19 mm (n=2, 2%), 21 mm (n=14, 12%), 23 mm (n=28, 25%), 25 mm (n=42, 37%), and 27 mm (n=27, 24%).
Annulus-to-coronary distance and coronary ostium size
Patients after VSRR had a significantly higher annulus-to-coronary distance for the right coronary artery (RCA; Bio-Bentall 12.5±5.4 mm vs VSRR 18.0±5.8 mm; p<0.001) and the left coronary artery (LCA; Bio-Bentall 8.0±4.5 mm vs VSRR 11.6±4.6 mm; p<0.001) compared to patients after a Bio-Bentall procedure. The ostium size of the RCA was slightly larger in patients after a Bio-Bentall procedure, compared with after VSRR, and reached statistical significance (Bio-Bentall 6.9±2.6 mm vs VSRR 6.4±2.0 mm; p=0.03), whereas there was no difference in the ostium size of the LCA (Bio-Bentall 7.7±2.3 mm vs VSRR 7.7±2.6 mm; p=0.9) (Table 2).
Table 2. Summary of the CT measurements of the annulus area and coronary ostium height and size.
| VSRR n=250 | Bio-Bentall n=113 | p-value | |
|---|---|---|---|
| Annulus area, mm2 | 661±108 | 385±78 | <0.001 |
| Annulus-to-coronary distance, mm | RCA: 18.0±5.8 | RCA: 12.5±5.4 | <0.001 |
| LCA: 11.6±4.6 | LCA: 8.0±4.5 | <0.001 | |
| Coronary ostium size, mm | RCA: 6.4±2.0 | RCA: 6.9±2.6 | 0.03 |
| LCA: 7.7±2.6 | LCA: 7.7±2.3 | 0.9 | |
| Data are mean±standard deviation. CT: computed tomography; LCA: left coronary artery; RCA: right coronary artery; VSRR: valve-sparing root repair | |||
Annulus area
In the VSRR group, 12 out of 250 patients (4.8%) had an annulus area over 840 mm2 resulting in no option for a transcatheter valve replacement due to the lack of matching large valve prosthesis sizes. In Bio-Bentall patients, 14 out of 113 (12.4%) had an annulus area smaller than 300 mm2 necessitating the implantation of the smallest available transcatheter valves, such as the 20 mm SAPIEN 3 Ultra (Edwards Lifesciences), 20 mm Myval (Meril Life Sciences), or the 23 mm Evolut FX (Medtronic), in case of deterioration (Figure 4).
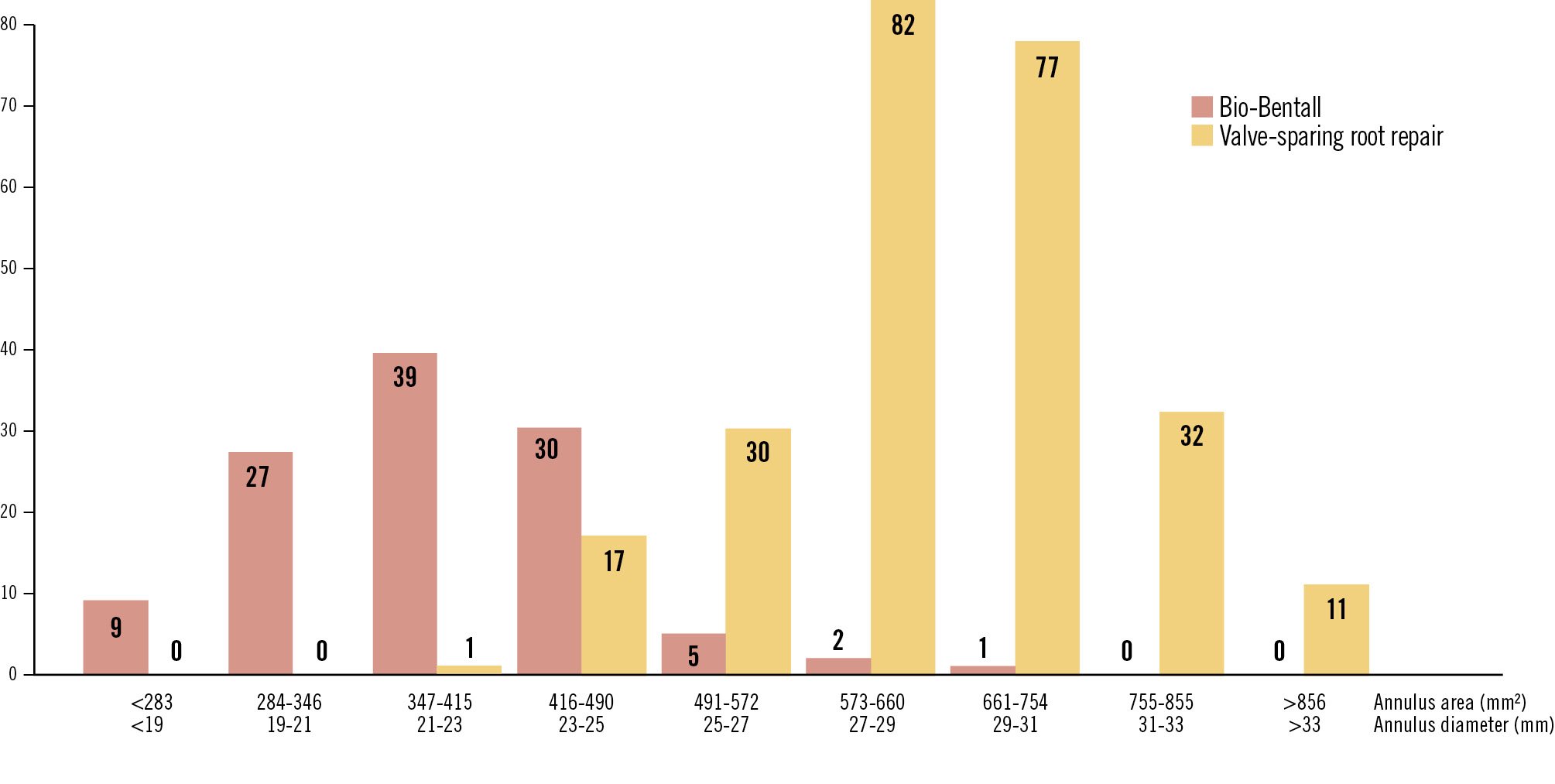
Figure 4. Annulus area. Annulus areas (mm2; x-axis) and annulus diameters (mm; x-axis) after Bio-Bentall (min. 237 mm2; max. 661 mm2) and valve-sparing root repair (min. 393 mm2; max. 1,163 mm2). The y-axis shows the number of patients (n).
Height of the coronary ostia after VSRR and Bio-Bentall procedures
After VSRR, the height of the coronary ostia was evaluated by using a standard 10 mm distance from the annulus to the lower rim of the ostium. The majority (61.6%, n=154) had the coronary ostia located above 10 mm, while almost one-third (29.2%, n=73) had one ostium partially below this threshold. Only 3.6% (n=9) of patients had both coronary ostia partially below the level of 10 mm. Twelve patients (4.8%) had one coronary ostium fully under 10 mm, and two patients (0.8%) had either both coronary ostia or one partially and one fully located below the threshold (Figure 5).
In the Bio-Bentall group, the reference point for the coronary height was the upper rim of the biological prosthesis, also known as the valve height. One-third of patients (n=36; 31.9%) had both coronary ostia above the valve height, while 26.5% (n=30) had one ostium partially below the valve height, and 4.4% (n=5) had both ostia partially below the threshold. Considering the higher-risk group for coronary obstruction, 23% (n=26) had one coronary ostium fully below the upper rim of the valve, while 8% (n=9) had one fully and one partially below the upper valve level, and 7 (6.2%) had both coronary ostia fully below the upper valve level (Figure 5).
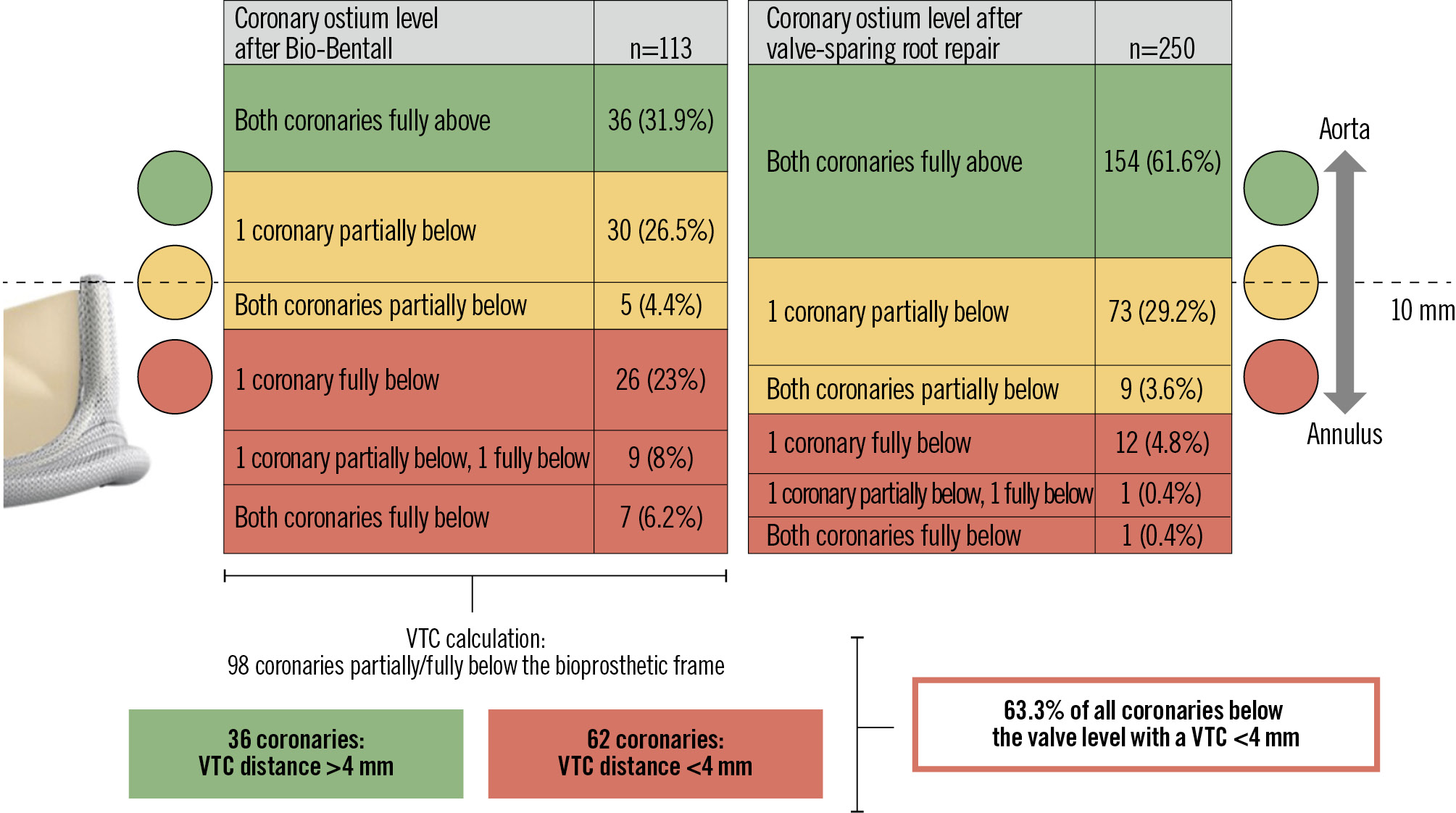
Figure 5. Height of the coronary ostia after Bio-Bentall and VSRR procedures. The standard reference after aortic root repair is defined by the distance of 10 mm from the annulus level to the lower rim of the coronary artery. After a Bio-Bentall procedure, the height of the coronary ostia is defined at three levels: below the level of the valve prosthesis, partially covered by the upper crown of the prosthesis, and above the valve prosthesis. When calculating the VTC after root replacement, 98 coronary arteries were found to be partially or fully below the valve level. The majority of 62 coronary ostia (63.3%) had a VTC below 4 mm. These 62 complex coronary locations were found in 37 patients who were assessed individually for valve-in-root TAVI±leaflet or coronary modification technique (Supplementary Figure 1). TAVI: transcatheter aortic valve implantation; VSRR: valve-sparing root repair; VTC: valve-to-coronary
Valve-to-coronary distance in patients after a Bio-Bentall procedure
In patients after a Bio-Bentall procedure with at least one coronary artery partially below the valve level, the VTC was analysed, for a total of 98 coronary ostia. This measurement has been defined as a risk factor for valve-in-root procedure, according to the Vancouver definition18, if the distance is below 4 mm. Out of the 98 coronary ostia, the VTC was higher than 4 mm in only 36 cases, whereas the majority (62 coronary ostia, 63.3%) had a VTC below 4 mm (Figure 5). The 62 coronary ostia at risk were found in 37 patients who were referred for a detailed evaluation by an experienced interventional cardiologist for a transcatheter valve-in-root option.
Technical options for patients at high risk for coronary obstruction
In the Bio-Bentall group, 37 patients were detected with a high risk of coronary obstruction due to the height of the coronary ostia either partially or fully below the valve level and a VTC below 4 mm. Out of these 37 patients, 21 were still considered suitable to receive a standard valve-in-root procedure, while 15 required some form of leaflet modification. One patient was unsuitable for transcatheter treatment and would have required a reoperation in case of a bioprosthetic failure (Supplementary Figure 1).
Impact of straight versus Valsalva graft on the VTC in Bio-Bentall patients
The VTC was assessed in the context of the implanted type of aortic prosthesis (Valsalva vs straight) and the size of the aortic graft. Out of the 113 Bio-Bentalls, 55 straight grafts and 16 Valsalva grafts were assessed regarding their effect on the VTC to the LCA. All patients belonged to the group in which at least one coronary ostium was partially below the valve level. A significant difference could be found in the VTC for the Valsalva graft of the LCA ostium with a larger distance of 4.95 (IQR 4.2-5.9) mm, in comparison to the straight graft (3.1 [IQR 2.3-4.2] mm; p<0.001). The regression analysis confirmed the Valsalva graft was a significant parameter, contributing to a higher VTC for the left coronary artery (LCA-VTC: odds ratio [OR] 3.4, 95% confidence interval [CI]: 1.47-7.88; p=0.0042), whereas the size of the aortic graft itself was not found to contribute to a higher VTC (OR 0.81, 95% CI: 0.61-1.07; p=0.13).
Discussion
This study underlines the importance of the initial procedure, especially for younger patients, as a cornerstone for lifetime management, including the possible need for TAVI after a VSRR or Bio-Bentall procedure. While risk assessment for simple ViV procedures exists18, there should equally be guidance for anatomical and surgical factors to facilitate a future valve-in-root treatment. In addition to a simple valve-in-root implantation, we assessed the feasibility of a complex transcatheter treatment in patients at risk of coronary obstruction by considering the most recent strategies such as coronary chimneys and the BASILICA manoeuvre.
Annulus area
We detected 4.8% of patients in the VSRR group with an annulus area over 840 mm2 who would currently not be able to undergo a valve-in-root procedure due to the lack of suitable transcatheter aortic prostheses. The cutoff is currently at an annulus area of 840 mm2 considering the largest transcatheter valve on the market (32 mm Myval). While overdilation with additional volume in the balloon is often utilised, this is outside of the indications for use. Active downsizing by choosing a smaller tube or Valsalva graft for VSRR might be an option in selected patients as long as the function of the repaired aortic valve is not compromised. On the contrary, 12.4% of patients in the Bio-Bentall group had annulus areas under 300 mm2, which may complicate a future transcatheter valve-in-root implantation and presents a high risk of PPM. The reported prevalence of severe PPM after ViV is very variable and depends on the type of transcatheter valve implanted, occurring in 6-39% for self-expanding valves and in 16-18% for balloon-expandable valves192021. Specifically for smaller transcatheter valves, higher gradients may be already expected during the initial TAVI procedure, ranging between 7 mmHg for self-expanding and 15 mmHg for balloon-expandable valves22. It could also be shown that moderate to severe PPM after TAVI in small annuli is more pronounced in the balloon-expandable group, with a rate of 35% after 30 days compared to 11% in the self-expanding group. This latter group also shows better haemodynamic results, specifically in the supra-annular position22. However, current evidence on TAVI in small annuli is limited to native aortic valves. Considering the number of patients in our cohort with an annular area of under 300 mm2 after a Bio-Bentall procedure (n=14), an individualised treatment approach − involving additional measures like the patient’s body surface area, clinical condition, and further CT information on the coronary ostium location and the aortic root anatomy − will be required in case future treatment is needed.
To overcome this problem, it is of utmost importance to implant a sufficiently large valve prosthesis that not only prevents PPM for the surgically implanted valve but also is sufficiently sized to allow for a ViV procedure without the risk of PPM. Apart from the risk of PPM, most recent long-term data on biological SAVR underline the importance of the implantation of a larger valve, as it is correlated with longer patient survival and improved valve durability23.
Coronary ostia height
Treatment planning for patients after a Bio-Bentall procedure requires the calculation of the risk of coronary obstruction, focusing on the height of the coronary ostia, which is defined as the distance between the annulus and the lower rim of the origin of the coronary artery. In cases where the ostial location is below the upper rim of the prosthesis, the VTC also needs to be considered. The analysis of both parameters in our Bio-Bentall cohort indicated a considerable number of patients in whom a future valve-in-root might be complicated, potentially resulting in the need for a leaflet or coronary modification technique.
Werner et al retrospectively analysed 64 patients who had undergone Bio-Bentall implantation, of whom 44 (68.8%) also received a Valsalva prosthesis. The results showed that more than half of these patients (56%) were at risk of coronary obstruction during a future valve-in-root procedure, with almost 19% having both coronary arteries at risk7. In the investigated cohort, nearly all patients (96.9%) had at least one coronary ostium below the level of the valve height. They also detected that the left coronary ostium was at risk of obstruction in almost one-third of the patients (29.7%), compared to only 10.9% at risk of obstruction for the RCA.
In our data, we first saw a difference between the two techniques, showing that after surgical mobilisation for VSRR, both coronary ostia are located significantly higher than in patients who underwent a Bio-Bentall procedure. In the Bio-Bentall group, 37% of patients had at least one coronary ostium fully below the valve level, potentially complicating a future valve-in-root option. This figure is considerably less than reported by Werner et al and may be related to differences in surgical techniques. The additional analysis of potential leaflet modification techniques in the patients at risk for coronary obstruction provides further information on the technical feasibility of performing an intervention instead of a reoperation, using the most recent methods. Based on local interventional experience, a coronary chimney procedure was considered as the method of choice for 7 patients due to the higher location of the coronary ostia, whereas 8 patients were candidates for the BASILICA manoeuvre, which is chosen in cases with a suitable distance between the implanted valve and the wall of the aortic root.
To our knowledge, the size of the coronary ostia and its importance has not been investigated or reported before and certainly contributes to the considerations during valve-in-root procedures. The clinical importance of larger coronary ostia reaching above the bioprosthetic stent frame might be a useful feature to prepare the patient at the time of surgery for a future valve-in-root procedure. This feature can be influenced to a certain degree by the surgeon.
The Valsalva graft and its impact on the VTC
Despite rather smaller numbers of patients that received a Valsalva graft, we found, in our cohort, an impact on the position of the LCA ostium relative to the valve resulting in a larger VTC and consequently facilitating a future valve-in-root procedure. The impact of the use of the Valsalva graft has been investigated by Brener et al in 81 CT scans of patients after a Bio-Bentall procedure24. Patients with straight aortic grafts or abnormal root anatomy experienced increased odds of complex valve-in-root TAVI, which was the case in about 50% of the patients. Interestingly, the measurements of the VTC between straight and Valsalva grafts did not differ in the study, but the relationship between the graft size and the implanted valve predicted the likelihood of a complex valve-in-root TAVI, specifically if the diameter equalled or exceeded 5 mm. In our analysis, we detected a beneficial effect of the Valsalva prosthesis resulting in a larger VTC to the LCA, regardless of the difference between the chosen graft and valve size.
Surgical considerations
The surgical considerations, based on the measurement results, are summarised in the Central illustration. We can draw four important conclusions regarding surgical considerations to facilitate a future valve-in-root procedure.
⢠First, the left coronary ostium should be mobilised in Bio-Bentall procedures in a similar fashion as in VSRR. Aortic root repair with the Tirone David technique, which requires full mobilisation of the root, may be the appropriate technique for adequate preparation of the left coronary ostium.
⢠Second, the choice of a Valsalva prosthesis seems to contribute effectively to the VTC, particularly with regard to the left coronary ostium. Therefore, to avoid the risk of coronary obstruction in future valve-in-root procedures, a Valsalva graft should be chosen over a straight prosthesis.
⢠Third, the repair techniques used in the David procedure should be adjusted to allow for a potential valve-in-root procedure in patients with a very large aortic annulus. In such cases, a pronounced reduction of the annulus may be required to facilitate a subsequent valve-in-root option.
⢠Fourth, in a Bio-Bentall procedure, the first valve prosthesis must be chosen considering the potential effect of PPM.
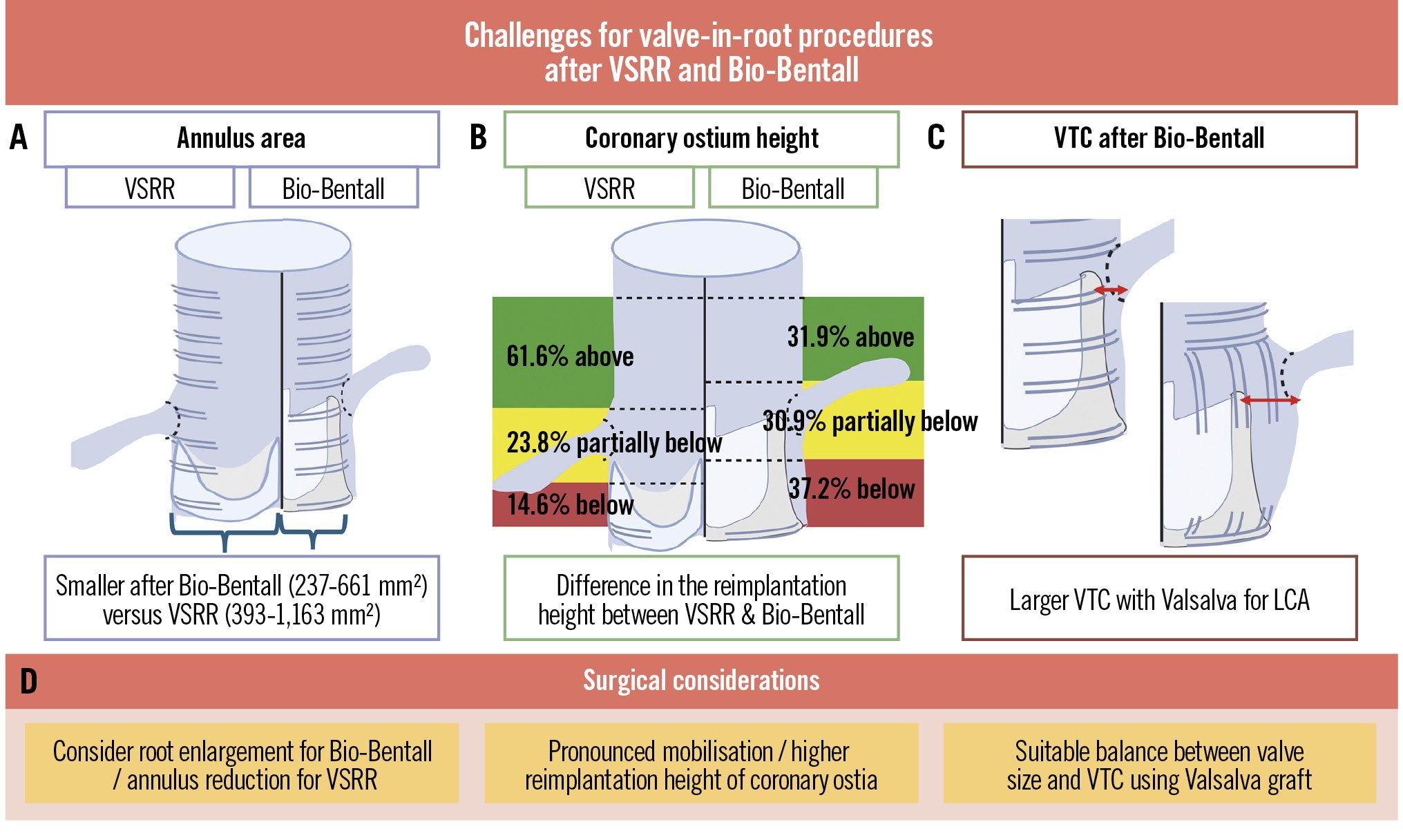
Central illustration. Challenges after VSRR and Bio-Bentall procedures and surgical solutions to facilitate future transcatheter treatment at the time of initial surgery. Anatomical considerations after VSRR and Bio-Bentall procedures: (A) aortic annulus area is significantly smaller after a Bio-Bentall than after a VSRR procedure; (B) difference in the coronary ostium height post-procedure; (C) a larger VTC can be achieved using a Valsalva graft for the LCA. D) Surgical considerations. The reduction of the annulus during VSRR may be considered as an individual treatment option by choosing a smaller Valsalva graft as long as the function of the aortic valve is not compromised. LCA: left coronary artery; VTC: valve-to-coronary distance; Valsalva: Valsalva aortic graft; VSRR: valve-sparing root repair
Limitations
Our study focuses on measurements in a cohort of patients that underwent VSRR and Bio-Bentall procedures over the last 12 years. The cohort size is limited by the number of patients who were retrospectively available for analysis because of the availability of postoperative CT scans. The data reflect a single-centre experience.
The CT measurements for the height of the coronary ostia, specifically in the VSRR group, use a 10 mm annulus-to-coronary distance as a benchmark. This measure was established for TAVI in native aortic valves some time ago25 and serves as an orientation point in clinical practice at our institution to distinguish between patients at risk for coronary obstruction and those who are at low or no risk. However, the 10 mm annulus-to-coronary distance is not the only parameter that can predict coronary obstruction, especially in the context of VSRR, where the native root is wrapped by the external graft and undergoes less vertical change. Sinus width, leaflet height, and leaflet-to-coronary distance are further parameters that require attention in selective cases and were not specifically analysed in this study2627.
Altogether, there were 5 patients in the Bio-Bentall cohort with a RESILIA INSPIRIS valve. This valve has an expandable frame, which might allow the implantation of a larger valve. However, there is a vascular prosthesis around the valve in this setting, which might reduce its ability to expand. We also did not take into account the possibility of a controlled ring fracture before valve-in-root, which could also be an option for an individualised transcatheter treatment.
Conclusions
The feasibility of a future valve-in-root procedure depends on the height of the coronary ostia and the choice of aortic valve and graft sizes. A Bio-Bentall procedure with the Valsalva graft shows a beneficial impact on the valve-to-coronary distance of the left coronary ostium. During the initial operation, surgeons should consider a high implantation level for the coronary ostia and a suitable valve-to-coronary distance to facilitate future valve-in-root options. The lifetime management of patients with aortic valve disease begins with the first procedure.
Impact on daily practice
Anatomical challenges exist after valve-sparing root repair or Bio-Bentall procedures when considering the feasibility of a transcatheter valve-in-root procedure in case of future valve deterioration. Crucial parameters that need to be taken into account for a future transcatheter treatment are the annulus area, the height of the coronary ostia, and the valve-to-coronary distance. During the initial surgical procedure, surgeons should aim for a high implantation of the coronary ostia as well as a suitable balance between the valve and vascular prosthesis size to achieve a sufficient valve-to-coronary distance to facilitate valve-in-root options, as lifetime management begins with the initial procedure.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.