Cory:
Unlock Your AI Assistant Now!
A 73-year-old female presented with a one-day history of chest pain associated with a peak troponin I of 87 ng/L. Her medical history included atrial fibrillation with prior pulmonary vein isolation, bioprosthetic aortic valve replacement, previous pacemaker implantation, and breast cancer in remission. A 12-lead electrocardiogram showed a right ventricular paced rhythm. An echocardiogram 8 months prior to index presentation showed a left ventricular ejection fraction of 49% with no overt regional wall motion abnormality. Given her current presentation, she was treated for acute coronary syndrome (ACS) and commenced dual antiplatelet therapy (DAPT). Subsequently, she underwent a coronary angiogram, which revealed a right-dominant circulation with only mild-to-moderate disease. Additionally, of relevance, the large obtuse marginal (OM) branch had a tortuous course. As there was no identifiable culprit lesion on angiography (Moving image 1), a decision was made to perform optical coherence tomography (OCT) of all major epicardial vessels. On passing the guidewire into the OM branch and undertaking the OCT pullback, angiography showed the vessel to be stenotic with tandem focal stenoses (Moving image 2), while OCT revealed intimal disruption overlying an attenuating plaque on OCT (Figure 1, Moving image 3). Additionally, the longitudinal OCT profile showed corresponding areas of focal protrusion. On withdrawal of the guidewire, the focal stenoses seen on angiography disappeared, suggesting a diagnosis of “concertina effect” (Figure 1)12. OCT examination of the left anterior descending and right coronary arteries revealed a fibrolipidic plaque with a thick fibrous cap, but it did not identify a culprit. The patient was therefore treated conservatively with DAPT and discharged with a plan for risk factor modification and clinical follow-up. Patients with ACS presenting without a culprit lesion pose major diagnostic and procedural challenges for the interventional cardiologist. Intracoronary imaging (ICI), preferably OCT, has been recommended to assist in ACS cases where angiography is ambiguous3. However, it is important to recognise that interpretation of ICI requires experience, and subsequent decision-making can be difficult. Our case represents the potential difficulty of engaging an ICI-guided approach, whereby a pseudostenosis, generated by wire-induced coronary concertina, resulted in OCT images suggestive of fibroatheroma with intimal disruption and plaque rupture. There was a risk that these findings could have been mistaken as a true culprit, and unnecessary stenting could have been pursued. Careful review of the OCT highlighted that the anomalies were limited to a few frames, with the vessel abruptly transitioning back to a normal architecture with circumferential visibility of the external elastic lamina (Figure 1, Supplementary Figure 1). The longitudinal plane is optimal for identifying a concertina effect, as the characteristic wrinkling or pleating is highly focal. Additionally, if the OCT pullback were performed over a stiff guidewire, consideration should be given to exchanging for a softer wire and repeating the acquisition. In our case, angiographic coregistration and resolution of the stenoses upon wire withdrawal aided interpretation. In conclusion, this case highlights the importance of reviewing all available information provided by angiography and ICI, thereby avoiding misinterpretation of isolated findings. 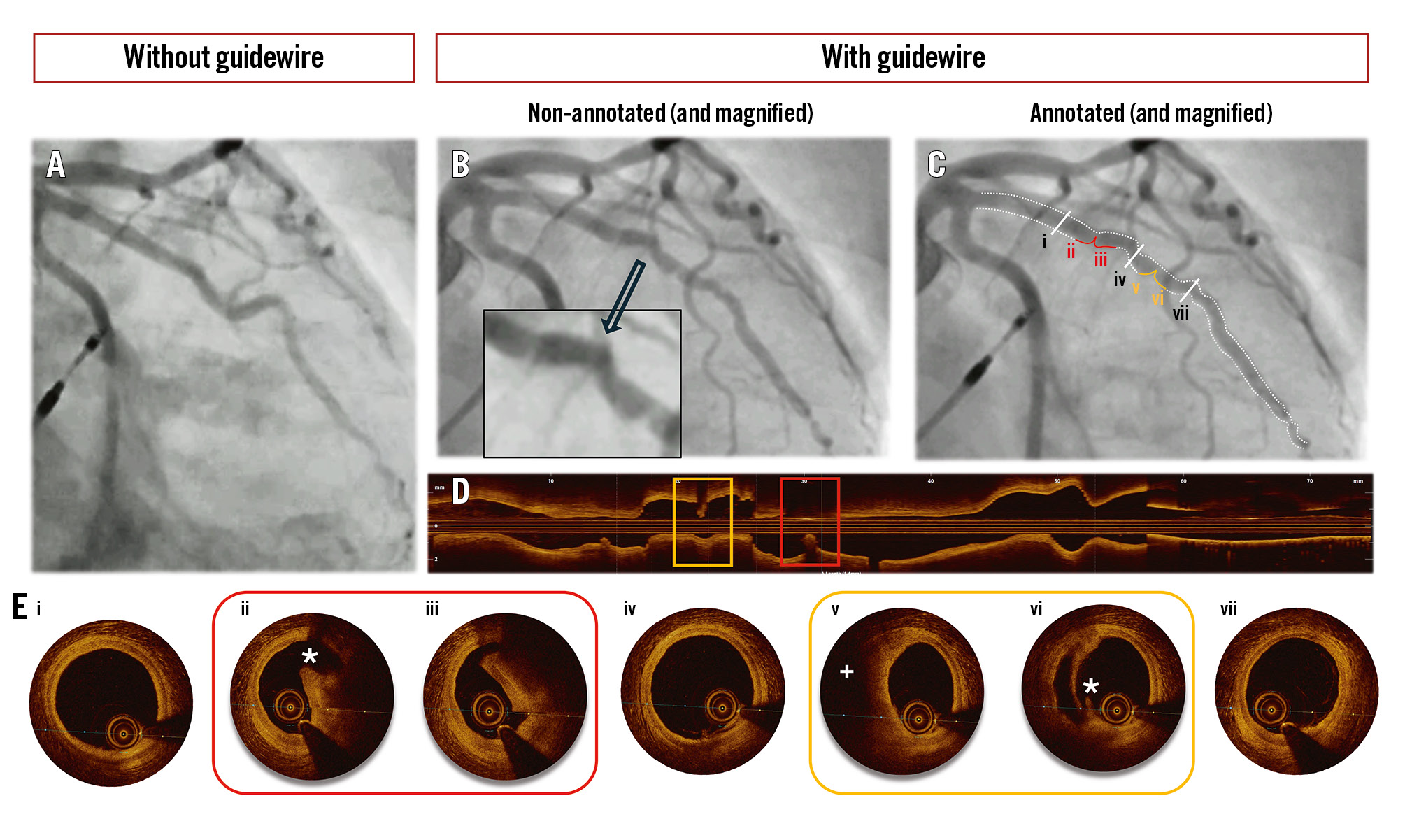
Figure 1. Concertina effect mimicking plaque rupture on OCT. Fluoroscopic images of the obtuse marginal branch taken before (A) and after (B) guidewire insertion. C) An annotated version of B displaying sequential OCT frames (i to vii) along the proximal to distal segment of the vessel. Additionally, the OCT cross-sections corresponding to C show the abrupt transition of normal lumen (i, iv, vii) to areas of focal stenosis with suggestion of plaque rupture. Furthermore, these sites appear pinched on the OCT longitudinal display (D). E) OCT cross-sections. OCT: optical coherence tomography
Conflict of interest statement
T.W. Johnson has received consultancy and speaker fees from Abbott, Boston Scientific, and Terumo; and has received an institutional research grant from Abbott Vascular. N. Chandra Mohan has received an institutional research grant from Abbott Vascular.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Fluoroscopic run demonstrating a large, tortuous unobstructed obtuse marginal branch.
Moving image 2. Evidence of tandem focal stenosis in the obtuse marginal branch after introduction of a guidewire.
Moving image 3. OCT pullback of the obtuse marginal branch reveals circumferential visualisation of the external elastic lamina, followed by an abrupt transition into regions showing features consistent with intimal disruption overlying fibroatheromatous plaque, observed over only a few frames. Data availability statement.